
Introduction
Wildfires don’t just burn through forests and homes—they release invisible toxins into the air, water, and soil that can harm the body.1,2,3
Understanding these toxins, their impact on your body, and how to aid your body’s ability to detox effectively is critical. Once you know how these toxins impact long-term health and know your exposure levels, you can take strategic steps to support your individual health as you move forward.
The Toxic Aftermath: What’s in Wildfire Smoke?
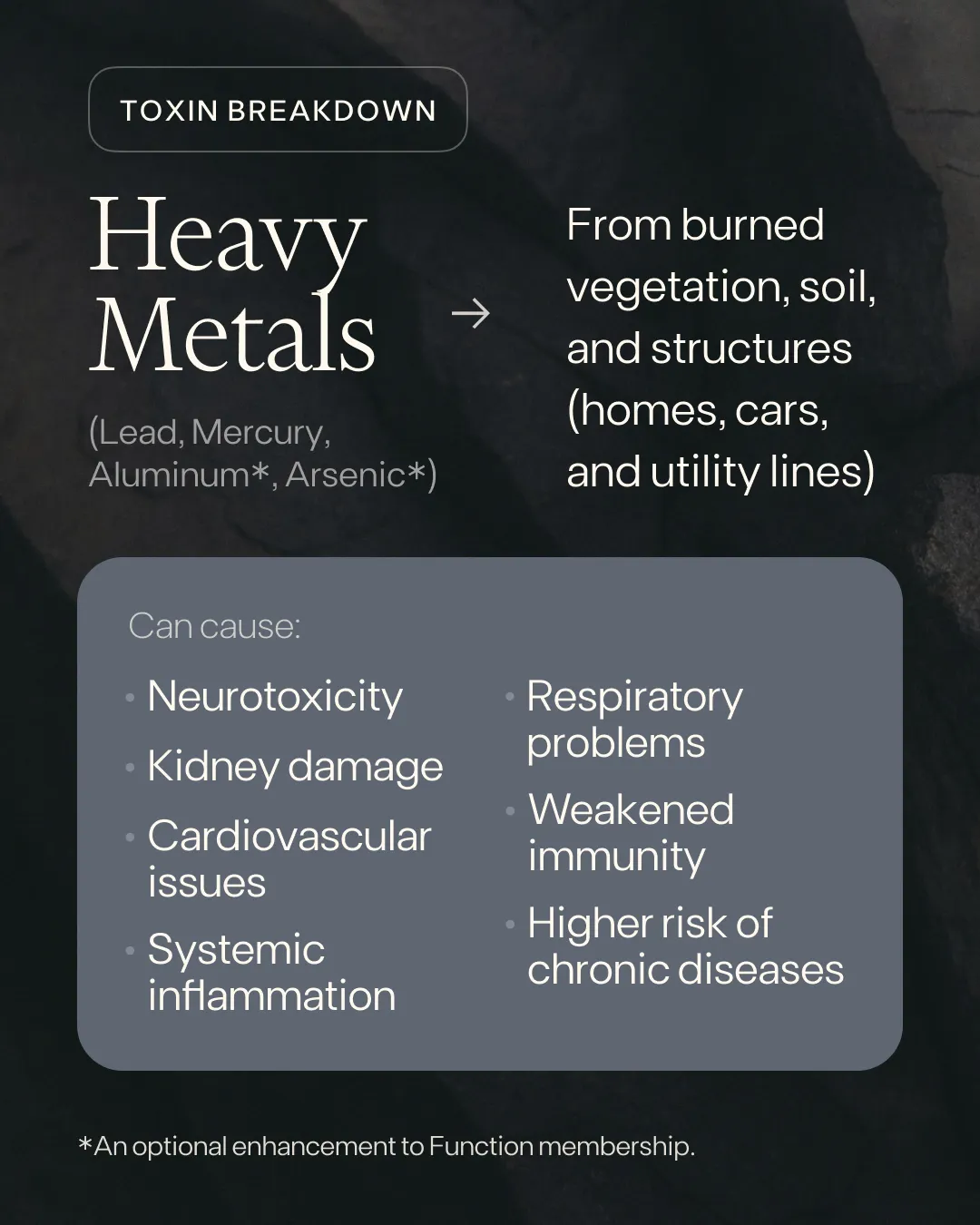
Heavy Metals: Neurotoxic and Inflammatory
What They Are
When vegetation, soil, homes, cars, and utility lines burn, heavy metals like lead, mercury, aluminum, and arsenic are released.4 These metals don’t just disappear after the fire—they settle into the environment and find their way into the body through inhalation or absorption.1,2
How They Impact the Body
Once inside, heavy metals can:
- Accumulate in tissues, disrupting neurological function5,6
- Damage kidneys7,8
- Increase cardiovascular disease risks9
- Trigger systemic inflammation10
- Weaken immunity11
- Impair respiratory health12
- Raise the risk of chronic disease13,14,15
How to Take Charge
Monitor your exposure by testing lead, mercury, aluminum, and arsenic. Then, take steps to support your liver and kidney health.
BPA: The Hormone Disruptor
What It Is
When plastics burn—including those in electronics and building materials—they release the chemical BPA into the air.16,17
How It Impacts the Body
Once inside, BPA mimics estrogen and disrupts hormone balance,18 increasing the risk of:
- Infertility19,20
- Insulin resistance21,22,23
- Developmental issues24,25
How to Take Charge
Support your body’s natural detoxification processes to help eliminate BPA and reduce its effects.

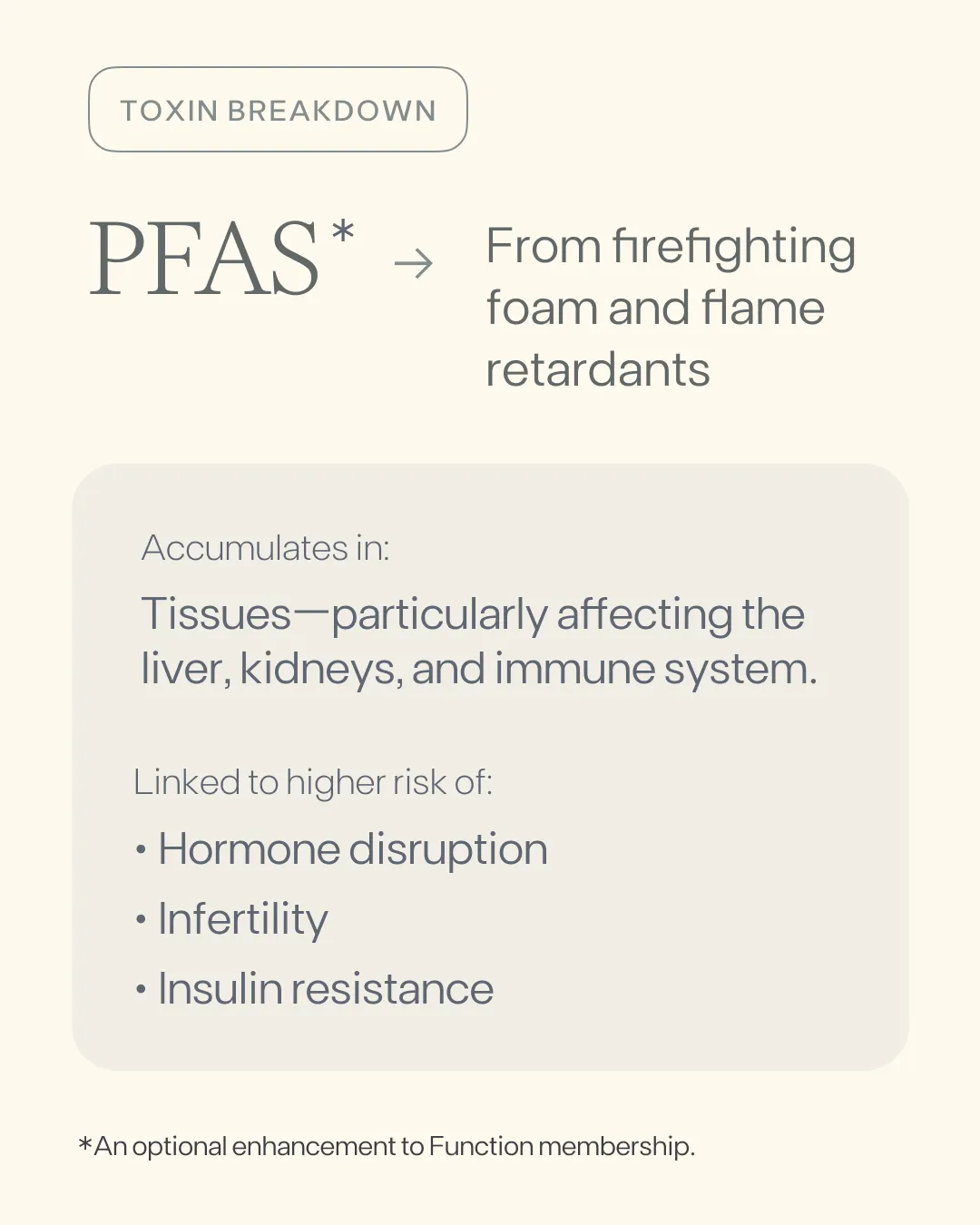
PFAS: The “Forever Chemicals”
What They Are
PFAS are chemicals commonly found in firefighting foam and flame retardants,26,27 and when released into the environment, they persist indefinitely.
How They Impact the Body
These chemicals can:
- Accumulate in the liver and kidneys28,29
- Affect the immune system30,31
- Increase the risk of hormone disruption32,33 and infertility34,35
- Increase the risk of metabolic disorders36,37
- Increase the risk of cancer38
How to Take Charge
Test for PFAS to gauge your exposure levels. Then, take action to help your body eliminate these persistent toxins.
How Toxins Attack Your Health
Once inhaled or absorbed, these toxins don’t just pass through—they stay. The result is oxidative stress,1 inflammation,10 and hormonal dysfunction32,33—which can increase disease risk,3,14,15 and long-term damage.7,8,38 But there are ways to counteract this damage and protect your health moving forward.43,44,45
.webp)
Action Steps to Support Your Body Post-Wildfire Exposure
While you can’t control if you’ve been exposed, you can decide what you do next. You have the power to protect and support your health—here’s how to take action:
1. Boost Antioxidant Defenses
Eat colorful, organic fruits, vegetables, leafy greens, nuts, and seeds to neutralize free radicals, reduce oxidative stress, and protect cells from toxin damage.39,40 Load up on cruciferous vegetables like broccoli, cauliflower, and kale, which contain sulforaphane to naturally improve glutathione levels.41,42
2. Support Your Liver and Kidneys
Consider supplementing with glutathione, milk thistle, or NAC (N-acetylcysteine) to support detoxification and help your body process harmful substances more efficiently.43,44,45 And remember to stay hydrated. Drink water and consume water-rich foods like cucumber, watermelon, and celery to support kidney function and waste elimination.46,47
3. Up Your Fiber
Incorporate fiber, especially soluble fiber, to bind to toxins in the digestive tract and promote their excretion.48,49 Chia seeds, flaxseeds, and leafy greens are great sources of fiber.
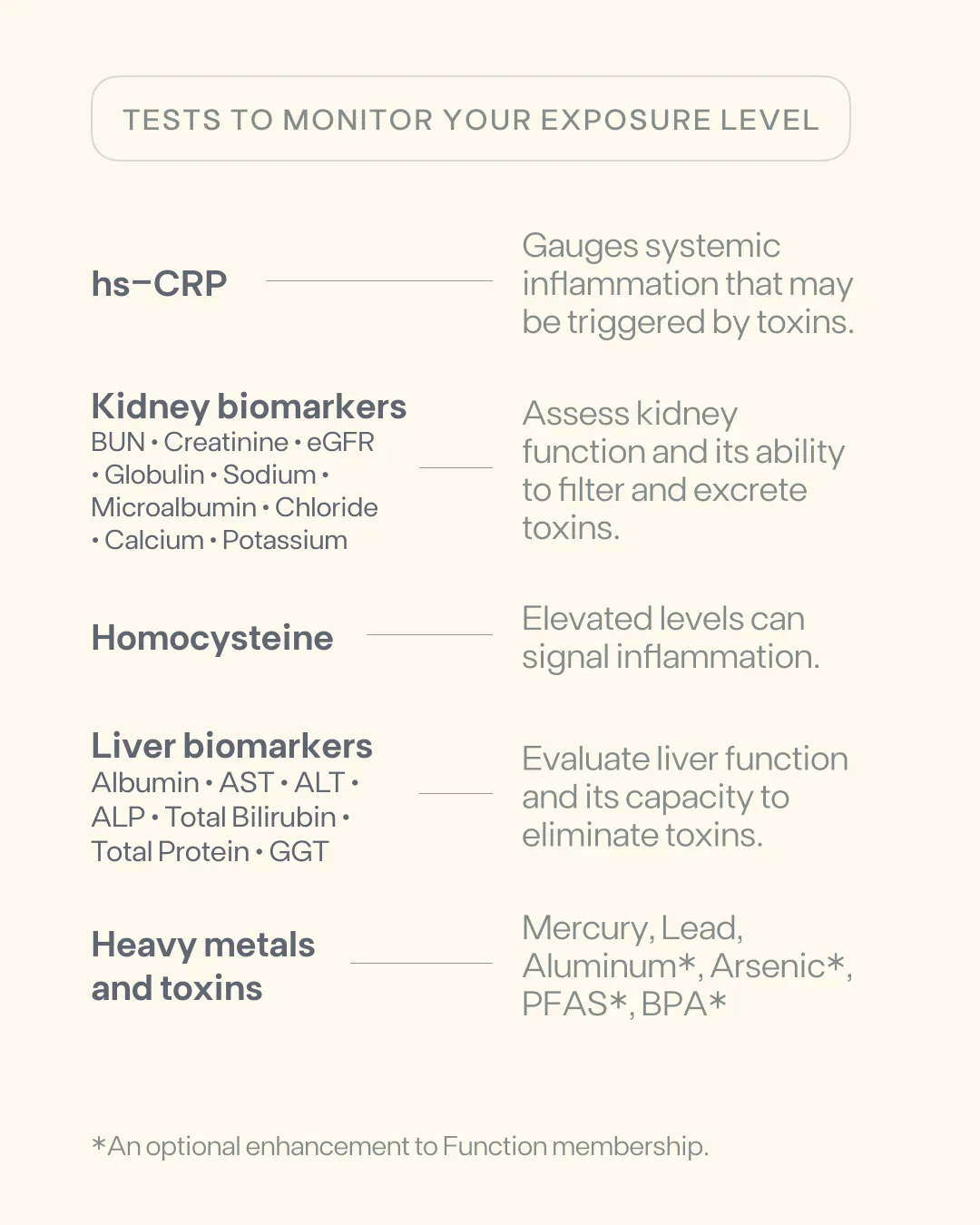
4. Test Your Exposure Levels
Wildfire toxins aren’t visible, but they leave an impact. Testing helps you understand your exposure and take intentional action for your health. And testing every 3-6 months means you can track improvements and adjust your health strategy as needed.
Function Health includes mercury and lead testing in its annual membership, and offers optional aluminum, arsenic, BPA, and PFAS testing to help gauge toxin levels. Biomarkers like hs-CRP50,51 and homocysteine52,53 measure systemic inflammation and oxidative stress, while liver and kidney tests provide insights into your body’s ability to process and eliminate toxins—all included in Function membership.54,55
5. Connect with Community to Reduce Stress
Health isn’t just physical. Social connection can play a powerful role in reducing inflammation and stress.56 Checking in on neighbors and reaching out to loved ones can contribute to resilience in the wake of stressful events like wildfires. Taking care of your health is easier when you have a strong support system.57
Why This Matters to Us

Function was born in LA. It’s the place that held us as this mission came to life. Watching wildfires devastate this place is personal, and we believe protecting health in the aftermath is just as important as putting out the flames.
LA County Firefighters: A Gift of Health
If you’re an LA County firefighter, we’re gifting you a Function membership and PFAS testing—because your health shouldn’t be the cost of service. Learn more and get your gifted Function membership here.
LA First Responders: Expanding Access
If you’re an LA first responder, we’re actively looking into ways to expand access. Share your contact info here to be the first to know if more gifted memberships become available. Thank you for your service.
Strengthening Your Health After Wildfires
Toxins don’t disappear when the smoke clears. They settle into bodies,1,2 disrupting hormones,32,33 immunity,30,31 and long-term health.7,8,38 But information is power, and taking the proper steps now can help mitigate the impact. Now’s the time to test, support your body’s ability to eliminate these toxins,43,44,45,48,49 and move forward with your health in focus.
Wildfires are beyond your control, but your health? You have a say in that. Be intentional and give your body what it needs to thrive after wildfire exposure.
1. Thangavel P, Park D, Lee YC. Recent insights into particulate matter (PM(2.5))-mediated toxicity in humans: an overview. Int J Environ Res Public Health. Jun 19 2022;19(12):7511. doi:10.3390/ijerph19127511
2. US EPA. Why Wildfire Smoke is a Health Concern. www.epa.gov. Published August 13, 2019. https://www.epa.gov/wildfire-smoke-course/why-wildfire-smoke-health-concern
3. Frumento D, Ștefan Țãlu. Effects of Wildfire Exposure on the Human Immune System. Fire. 2024;7(12):469-469. doi:https://doi.org/10.3390/fire7120469
4. Tchounwou PB, Yedjou CG, Patlolla AK, Sutton DJ. Heavy metal toxicity and the environment. Exp Suppl. 2012;101:133-164. doi:10.1007/978-3-7643-8340-4_6
5. Wang H, Matsushita MT. Heavy metals and adult neurogenesis. Curr Opin Toxicol. 2021;26:14-21. doi:10.1016/j.cotox.2021.03.006
6. Li B, Xia M, Zorec R, Parpura V, Verkhratsky A. Astrocytes in heavy metal neurotoxicity and neurodegeneration. Brain Research. 2021;1752:147234. doi:https://doi.org/10.1016/j.brainres.2020.147234
7. Pan S, Niu Y, Duan S, et al. Uric acid mediates the relationship between mixed heavy metal exposure and renal function in older adult people. Front Public Health. 2024;12:1403878. doi:10.3389/fpubh.2024.1403878
8. Lentini P, Zanoli L, Granata A, Signorelli SS, Castellino P, Dellaquila R. Kidney and heavy metals - The role of environmental exposure. Molecular Medicine Reports. 2017;15(5):3413-3419. doi:https://doi.org/10.3892/mmr.2017.6389
9. Yang AM, Lo K, Zheng TZ, et al. Environmental heavy metals and cardiovascular diseases: status and future direction. Chronic Dis Transl Med. Dec 2020;6(4):251-259. doi:10.1016/j.cdtm.2020.02.005
10. Wang Y, Wang Y, Li R, et al. Low-grade systemic inflammation links heavy metal exposures to mortality: A multi-metal inflammatory index approach. Sci Total Environ. 2024;947(174537):174537. doi:10.1016/j.scitotenv.2024.174537
11. Zhang H, Wang J, Zhang K, et al. Association between heavy metals exposure and persistent infections: the mediating role of immune function. Front Public Health. 2024;12:1367644. doi:10.3389/fpubh.2024.1367644
12. Rajkumar V, Gupta V. Heavy Metal Toxicity. PubMed. Published 2020. https://www.ncbi.nlm.nih.gov/books/NBK560920/
13. Pan Z, Gong T, Liang P. Heavy metal exposure and cardiovascular disease. Circ Res. 2024;134(9):1160-1178. doi:10.1161/CIRCRESAHA.123.323617
14. Cortés S, Zúñiga-Venegas L, Pancetti F, et al. A positive relationship between exposure to heavy metals and development of chronic diseases: A case study from Chile. Int J Environ Res Public Health. 2021;18(4):1419. doi:10.3390/ijerph18041419
15. Balali-Mood M, Naseri K, Tahergorabi Z, Khazdair MR, Sadeghi M. Toxic Mechanisms of Five Heavy Metals: Mercury, Lead, Chromium, Cadmium, and Arsenic. Frontiers in Pharmacology. 2021;12(643972). doi:https://doi.org/10.3389/fphar.2021.643972
16. Vasiljevic T, Harner T. Bisphenol A and its analogues in outdoor and indoor air: Properties, sources and global levels. Science of The Total Environment. 2021;789:148013. doi:https://doi.org/10.1016/j.scitotenv.2021.148013
17. Campanale C, Massarelli C, Savino I, Locaputo V, Uricchio VF. A Detailed Review Study on Potential Effects of Microplastics and Additives of Concern on Human Health. International Journal of Environmental Research and Public Health. 2020;17(4):1212. doi:https://doi.org/10.3390/ijerph17041212
18. Hafezi SA, Abdel-Rahman WM. The endocrine disruptor bisphenol A (BPA) exerts a wide range of effects in carcinogenesis and response to therapy. Curr Mol Pharmacol. 2019;12(3):230-238. doi:10.2174/1874467212666190306164507
19. Ziv-Gal A, Flaws JA. Evidence for bisphenol A-induced female infertility: a review (2007-2016). Fertil Steril. 2016;106(4):827-856. doi:10.1016/j.fertnstert.2016.06.027
20. Castellini C, Totaro M, Parisi A, et al. Bisphenol A and male fertility: Myths and realities. Front Endocrinol (Lausanne). 2020;11:353. doi:10.3389/fendo.2020.00353
21. Pérez-Bermejo M, Mas-Pérez I, Murillo-Llorente MT. The Role of the Bisphenol A in Diabetes and Obesity. Biomedicines. 2021;9(6):666. doi:https://doi.org/10.3390/biomedicines9060666
22. Wang T, Li M, Chen B, et al. Urinary Bisphenol A (BPA) Concentration Associates with Obesity and Insulin Resistance. The Journal of Clinical Endocrinology & Metabolism. 2012;97(2):E223-E227. doi:https://doi.org/10.1210/jc.2011-1989
23. Savastano S, Tarantino G, D’Esposito V, et al. Bisphenol-A plasma levels are related to inflammatory markers, visceral obesity and insulin-resistance: a cross-sectional study on adult male population. Journal of Translational Medicine. 2015;13(1). doi:https://doi.org/10.1186/s12967-015-0532-y
24. Nayan NM, Husin A, Siran R. The risk of prenatal bisphenol A exposure in early life neurodevelopment: Insights from epigenetic regulation. Early Human Development. 2024;198:106120. doi:https://doi.org/10.1016/j.earlhumdev.2024.106120
25.Grohs MN, Reynolds JE, Liu J, et al. Prenatal maternal and childhood bisphenol a exposure and brain structure and behavior of young children. Environmental Health. 2019;18(1). doi:https://doi.org/10.1186/s12940-019-0528-9
26. Fenton SE, Ducatman A, Boobis A, et al. Per‐ and polyfluoroalkyl substance toxicity and human health review: Current state of knowledge and strategies for informing future research. Environmental Toxicology and Chemistry. 2020;40(3):606-630. doi:https://doi.org/10.1002/etc.4890
27. Mazumder NUS, Hossain MT, Jahura FT, et al. Firefighters’ exposure to per-and polyfluoroalkyl substances (PFAS) as an occupational hazard: A review. Frontiers in Materials. 2023;10. doi:https://doi.org/10.3389/fmats.2023.1143411
28. Zhang X, Zhao L, Ducatman A, et al. Association of per- and polyfluoroalkyl substance exposure with fatty liver disease risk in US adults. JHEP Rep. May 2023;5(5):100694. doi:10.1016/j.jhepr.2023.100694
29. Shearer JJ, Callahan CL, Calafat AM, et al. Serum concentrations of per- and polyfluoroalkyl substances and risk of renal cell carcinoma. J Natl Cancer Inst. 2021;113(5):580-587. doi:10.1093/jnci/djaa143
30. Bline AP, DeWitt JC, Kwiatkowski CF, Pelch KE, Reade A, Varshavsky JR. Public health risks of PFAS-related immunotoxicity are real. Curr Environ Health Rep. Jun 2024;11(2):118-127. doi:10.1007/s40572-024-00441-y
31. Ehrlich V, Bil W, Vandebriel R, et al. Consideration of pathways for immunotoxicity of per- and polyfluoroalkyl substances (PFAS). Environmental Health. 2023;22(1). doi:https://doi.org/10.1186/s12940-022-00958-5
32. Li L, Guo Y, Ma S, Wen H, Li Y, Qiao J. Association between exposure to per- and perfluoroalkyl substances (PFAS) and reproductive hormones in human: A systematic review and meta-analysis. Environmental research. 2024;241:117553-117553. doi:https://doi.org/10.1016/j.envres.2023.117553
33. Lee JE, Choi K. Perfluoroalkyl substances exposure and thyroid hormones in humans: epidemiological observations and implications. Ann Pediatr Endocrinol Metab. Mar 2017;22(1):6-14. doi:10.6065/apem.2017.22.1.6
34. Rickard BP, Rizvi I, Fenton SE. Per- and poly-fluoroalkyl substances (PFAS) and female reproductive outcomes: PFAS elimination, endocrine-mediated effects, and disease. Toxicology. 2022;465:153031. doi:https://doi.org/10.1016/j.tox.2021.153031
35.Calvert L, Green MP, De Iuliis GN, et al. Assessment of the Emerging Threat Posed by Perfluoroalkyl and Polyfluoroalkyl Substances to Male Reproduction in Humans. Frontiers in Endocrinology. 2022;12. doi:https://doi.org/10.3389/fendo.2021.799043
36. Sun Q, Zong G, Valvi D, Nielsen F, Coull B, Grandjean P. Plasma Concentrations of Perfluoroalkyl Substances and Risk of Type 2 Diabetes: A Prospective Investigation among U.S. Women. Environmental Health Perspectives. 2018;126(3):037001. doi:https://doi.org/10.1289/ehp2619
37. Chen Z, Yang T, Walker DI, et al. Dysregulated lipid and fatty acid metabolism link perfluoroalkyl substances exposure and impaired glucose metabolism in young adults. Environment International. 2020;145:106091. doi:https://doi.org/10.1016/j.envint.2020.106091
38. Li S, Oliva P, Zhang L, et al. Associations between per-and polyfluoroalkyl substances (PFAS) and county-level cancer incidence between 2016 and 2021 and incident cancer burden attributable to PFAS in drinking water in the United States. Journal of Exposure Science & Environmental Epidemiology. Published online January 9, 2025. doi:https://doi.org/10.1038/s41370-024-00742-2
39. Carlsen MH, Halvorsen BL, Holte K, et al. The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutr J. 2010;9(1):3. doi:10.1186/1475-2891-9-3
40. Pruteanu LL, Bailey DS, Grădinaru AC, Jäntschi L. The Biochemistry and Effectiveness of Antioxidants in Food, Fruits, and Marine Algae. Antioxidants. 2023;12(4):860. doi:https://doi.org/10.3390/antiox12040860
41. Hodges RE, Minich DM. Modulation of metabolic detoxification pathways using foods and food-derived components: A scientific review with clinical application. J Nutr Metab. 2015;2015:760689. doi:10.1155/2015/760689
42. Cascajosa-Lira A, Prieto AI, Pichardo S, Jos A, Cameán AM. Protective effects of sulforaphane against toxic substances and contaminants: A systematic review. Phytomedicine. 2024;130:155731-155731. doi:https://doi.org/10.1016/j.phymed.2024.155731
43. Richie JP, Nichenametla S, Neidig W, et al. Randomized controlled trial of oral glutathione supplementation on body stores of glutathione. European Journal of Nutrition. 2014;54(2):251-263. doi:https://doi.org/10.1007/s00394-014-0706-z
44. Gillessen A, Schmidt HHJ . Silymarin as Supportive Treatment in Liver Diseases: A Narrative Review. Advances in Therapy. 2020;37(4):1279-1301. doi:https://doi.org/10.1007/s12325-020-01251-y
45. Ntamo Y, Ziqubu K, Chellan N, et al. Drug-induced liver injury: Clinical evidence of N-Acetyl cysteine protective effects. Oxid Med Cell Longev. 2021;2021(1):3320325. doi:10.1155/2021/3320325
46. Popkin BM, D'Anci KE, Rosenberg IH. Water, hydration, and health. Nutr Rev. Aug 2010;68(8):439-458. doi:10.1111/j.1753-4887.2010.00304.x
47. Liska D, Mah E, Brisbois T, Barrios PL, Baker LB, Spriet LL. Narrative Review of Hydration and Selected Health Outcomes in the General Population. Nutrients. 2019;11(1):70. doi:https://doi.org/10.3390/nu11010070
48. Kieffer DA, Martin RJ, Adams SH. Impact of dietary fibers on nutrient management and detoxification organs: Gut, liver, and kidneys. Adv Nutr. 2016;7(6):1111-1121. doi:10.3945/an.116.013219
49. Ke G, Yao Z, Yang T. Intestinal microbiota-mediated dietary fiber bioavailability. Frontiers in Nutrition. 2022;9. doi:https://doi.org/10.3389/fnut.2022.1003571
50. Sirivarasai J, Wananukul W, Kaojarern S, et al. Association between inflammatory marker, environmental lead exposure, and glutathione S-transferase gene. BioMed Research International. 2013;2013:474963. doi:https://doi.org/10.1155/2013/474963
51. Li Y, Rittenhouse-Olson K, Scheider WL, Mu L. Effect of particulate matter air pollution on C-reactive protein: a review of epidemiologic studies. Reviews on Environmental Health. 2012;27(2-3). doi:https://doi.org/10.1515/reveh-2012-0012
52. Min JY, Lee KJ, Park JB, Min KB. Perfluorooctanoic acid exposure is associated with elevated homocysteine and hypertension in US adults. Occupational and Environmental Medicine. 2012;69(9):658-662. doi:https://doi.org/10.1136/oemed-2011-100288
53. Ledda C, Cannizzaro E, Lovreglio P, et al. Exposure to Toxic Heavy Metals Can Influence Homocysteine Metabolism? Antioxidants. 2019;9(1):30. doi:https://doi.org/10.3390/antiox9010030
54.Sen P, Qadri S, Luukkonen PK, et al. Exposure to environmental contaminants is associated with altered hepatic lipid metabolism in non-alcoholic fatty liver disease. Journal of Hepatology. 2022;76(2):283-293. doi:https://doi.org/10.1016/j.jhep.2021.09.039
55. Pan S, Niu Y, Duan S, et al. Uric acid mediates the relationship between mixed heavy metal exposure and renal function in older adult people. Front Public Health. 2024;12:1403878. doi:10.3389/fpubh.2024.1403878
56. Uchino BN, Trettevik R, Kent de Grey RG, Cronan S, Hogan J, Baucom BRW. Social support, social integration, and inflammatory cytokines: A meta-analysis. Health Psychol. 2018;37(5):462-471. doi:10.1037/hea0000594
57. Holt-Lunstad J, Smith TB, Layton JB. Social Relationships and Mortality Risk: a Meta-analytic Review. PLoS Medicine. 2010;7(7). doi:https://doi.org/10.1371/journal.pmed.1000316
Related articles
Related articles
What could cost you $15,000 is $499
Function membership
$42
As someone navigating an autoimmune condition, it's been such a relief to finally have a clear, visual way to track what’s going on in my body—and actually understand it.

Early detection has given me this amazing gift of extra years, probably extra decades, with my family.
After 10 years of dealing with a health issue, 5 years of trying to get doctors to run more in-depth tests, Function finally helped me uncover the root cause.



