
Why it matters?
Electrolytes are essential minerals that regulate hydration, nerve function, muscle contractions, and pH balance. An imbalance can lead to symptoms ranging from fatigue and muscle cramps to life-threatening conditions like seizures or cardiac arrest. Recognizing and addressing these imbalances is crucial for maintaining overall health and preventing serious complications.
The vital role of electrolytes
Electrolytes are the unsung heroes of your body’s functionality. These essential minerals—sodium, potassium, calcium, magnesium, and chloride—regulate hydration, nerve signaling, muscle contractions, and pH balance. But when their levels get tipped out of balance, the consequences can range from mild fatigue to life-threatening complications like seizures or difficulty breathing.
Understanding the symptoms of electrolyte imbalance, root causes, and best ways to restore equilibrium is critical for maintaining energy, focus, and overall health. Whether you’re an athlete, someone managing a chronic illness, or simply looking to sustain good health, electrolyte balance is fundamental.
What is an electrolyte imbalance?
Your body is an electrochemical system, and electrolytes are the conductors. They keep your heart beating, your muscles contracting, and your brain firing. An electrolyte imbalance occurs when these minerals become too high or too low, throwing off crucial body processes. Even small shifts in levels can cause noticeable symptoms, like fatigue, muscle spasms, irregular heart rhythms, and confusion.
The role of key electrolytes
Each electrolyte plays a unique role in maintaining balance and supporting essential body functions:
- Sodium: Regulates fluid balance in cells and supports proper nerve signaling.
- Potassium: Essential for heart health, muscle and nerve function, and nutrient transport into cells.
- Chloride: Helps maintain blood pressure and pH balance in the body.
- Calcium: Helps contract smooth muscles, supports bone health and influences hormone signaling.
- Magnesium: Vital for nerve function, muscle relaxation, and blood pressure regulation.
- Carbon dioxide: Helps to balance the pH of the body.
A disruption in any of these electrolytes can lead to significant health consequences, affecting everything from cognitive function to cardiovascular stability.
Your body’s demand for electrolytes is constant, but lifestyle habits, chronic conditions, and even the environment can deplete them. Knowing how to fix electrolyte imbalances at home and take action can mean the difference between feeling sluggish and feeling your best.
What happens when you're low
Low electrolyte levels compromise your body’s ability to function. The results? Dehydration, dizziness, weakness, and even organ failure in extreme cases. Your cells struggle to maintain proper hydration, nerve signals falter, and muscles lose their ability to contract smoothly. If you’ve ever experienced cramps after intense exercise or felt fatigued after a long day in the sun, your electrolyte levels likely took a hit.
How does a major electrolyte imbalance impact long-term health?
When left untreated, severe electrolyte imbalances can cause seizures, coma, kidney failure, or cardiac arrest. That is why recognizing signs and symptoms of electrolyte imbalance early and correcting deficiencies or excess quickly is vital.
Major signs of imbalance
Electrolyte imbalances don’t just affect one system—they disrupt the whole body. Here’s what to watch for:
- Muscle cramps, spasms, or weakness - Low levels of electrolytes like magnesium or potassium can trigger painful muscle contractions, weakness, or spasms.
- Nausea and vomiting - Low potassium levels can impair muscle function in the gastrointestinal tract, which can cause nausea, vomiting, and intestinal paralysis.
- Confusion or irritability - Low sodium levels can cause brain swelling, leading to neurological symptoms like confusion, headaches, and brain fog.
- Fatigue or dizziness - When electrolyte levels drop, nerve signaling, muscle function, and blood pressure regulation are all impaired—leaving you feeling weak, sluggish, and dizzy.
- Headaches - Fluctuations in sodium and hydration levels can lead to headaches.
- Irregular heartbeat (arrhythmia) - Electrolytes like potassium, calcium, and magnesium help regulate heart rhythm. Imbalances can cause arrhythmias (irregular heart beat) and you may feel heart palpitations.
- Numbness or tingling - Deficiencies in calcium, potassium, or magnesium can interfere with nerve conduction, leading to a pins-and-needles sensation in the limbs, fingers, and toes.
- Diarrhea or constipation - Electrolyte imbalances can impact digestion, leading to irregular bowel movements. Low potassium can slow gut motility causing constipation, while imbalances in sodium and chloride can trigger diarrhea.
If you’re experiencing multiple symptoms, don’t ignore them—imbalances can escalate quickly. If you often experience these symptoms but aren’t sure why, connect with your healthcare provider and consider getting your electrolyte levels checked.
What causes imbalance?
Electrolyte levels don’t just drop for no reason. Identifying the root cause is key to preventing future imbalances.
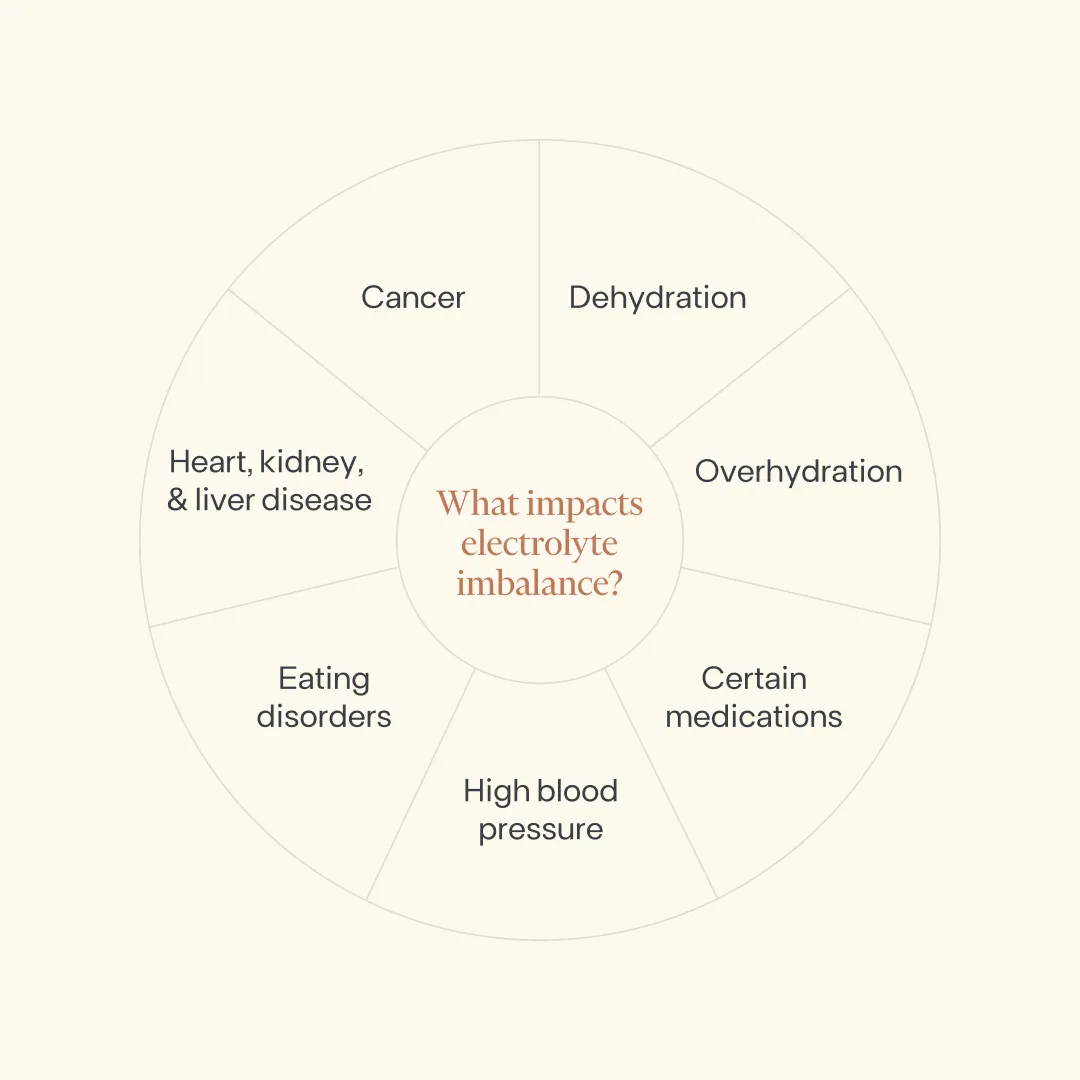
- Dehydration - This can occur from excessive sweating, vomiting, or diarrhea or simply not drinking enough water.
- Overhydration - Yes, drinking too much water can be a problem too—it can dilute sodium levels in your blood.
- Medications - Some medications can alter electrolyte levels—including diuretics, laxatives, antibiotics, and corticosteroids.
- Eating disorders - Prolonged fasting, purging, or laxative abuse can lead to drastic drops in sodium and potassium.
- Heart, Kidney, or Liver Disease - These conditions interfere with the body’s ability to regulate electrolytes, making imbalances more likely.
- Cancer - Electrolyte disorders are common in people with cancer, and chemotherapy treatments may worsen this.
How to fix it at home
When electrolyte levels drop, restoring balance should be your priority. Here’s how to correct electrolyte imbalance effectively:
1. Hydrate smart
Water alone won’t always cut it. To replenish lost minerals, look to coconut water, electrolyte powders, or homemade, natural electrolyte drinks (think lemon juice, sea salt, and honey in water). Keep in mind some pre-made electrolyte-infused beverages may be high in sugar, so check labels before purchasing or opt to make your own version at home.
2. Eat mineral-rich foods
Choose whole, nutrient-dense foods to ensure you’re getting the minerals you need.
Natural sources of potassium
The following foods are abundant in potassium:
- Lentils
- Squash
- Kidney beans
- Soybeans
- Bananas
Natural sources of calcium
These foods are high in calcium:
- Sardines
- Soy milk
- Organic tofu
- Salmon
- Soybeans
Natural sources of sodium
Choose these foods to support sodium levels:
- Fish
- Mussels
- Oysters
- Seaweed
- Himalayan pink salt & Celtic sea salt
Natural sources of chloride
Look for these foods to support healthy chloride levels:
- Seaweed
- Leafy greens
- Tomatoes
- Celery
- Lettuce
Natural sources of magnesium
Turn to these food staples to boost magnesium levels:
- Pumpkin seeds
- Chia seeds
- Almonds
- Spinach
- Cashews
3. Avoid excessively sugary drinks, alcohol, & caffeinated beverages
Sugary drinks can lead to further electrolyte imbalance while alcohol and caffeine can cause further dehydration.
4. Know when to seek medical help
Severe symptoms like heart palpitations, confusion, or persistent nausea and vomiting require immediate medical attention. If a healthcare provider identifies an electrolyte imbalance, treatment may include oral rehydration drinks, IV fluids, medications, or supplements to balance levels.
Takeaway
Electrolytes dictate how well your body functions. When levels drop, energy levels crash, nerves misfire, muscles spasm, and your brain slows down. The fix? Proactive hydration, a whole, nutrient-dense diet, and awareness of how lifestyle choices affect electrolyte balance.
Addressing electrolyte imbalance isn’t just about getting rid of muscle cramps or fatigue—it’s about supporting your everyday health. By making simple changes to your hydration routine and diet, you can ensure your body functions at its best, day in and day out.
Monitor your electrolyte levels over time as part of 100+ lab tests included in Function membership.
- Shrimanker I, Bhattarai S. Electrolytes. National Library of Medicine. Published July 24, 2023. https://www.ncbi.nlm.nih.gov/books/NBK541123/
- Cleveland Clinic. Electrolytes: Types, Purpose and Normal Levels. Cleveland Clinic. Published September 24, 2021. https://my.clevelandclinic.org/health/diagnostics/21790-electrolytes
- Urso C, Brucculeri S, Caimi G. Acid–base and electrolyte abnormalities in heart failure: pathophysiology and implications. Heart Failure Reviews. 2015;20(4):493-503. doi:https://doi.org/10.1007/s10741-015-9482-y
- Cleveland Clinic. Electrolyte imbalance. Cleveland Clinic. Published August 13, 2022. https://my.clevelandclinic.org/health/symptoms/24019-electrolyte-imbalance
- Drake TM, Gupta V. Calcium. PubMed. Published 2020. https://www.ncbi.nlm.nih.gov/books/NBK557683/
- Hafen BB, Burns B, Shook M. Anatomy, Smooth Muscle. PubMed. Published July 17, 2023. https://www.ncbi.nlm.nih.gov/books/NBK532857/
- National Institutes of Health. Magnesium. National Institutes of Health. Published June 2, 2022. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/
- Chen F, Wang J, Cheng Y, et al. Magnesium and Cognitive Health in Adults: A Systematic Review and Meta-Analysis. Advances in Nutrition (Bethesda, Md). 2024;15(8):100272. doi:https://doi.org/10.1016/j.advnut.2024.100272
- Oliveira RA, Sierra APR, Benetti M, et al. Impact of Hot Environment on Fluid and Electrolyte Imbalance, Renal Damage, Hemolysis, and Immune Activation Postmarathon. Oxidative Medicine and Cellular Longevity. 2017;2017:1-11. doi:https://doi.org/10.1155/2017/9824192
- Dhondup T, Qian Q. Acid-Base and Electrolyte Disorders in Patients with and without Chronic Kidney Disease: An Update. Kidney Diseases. 2017;3(4):136-148. doi:https://doi.org/10.1159/000479968
- Cleveland Clinic. Hyponatremia. Cleveland Clinic. Published 2022. https://my.clevelandclinic.org/health/diseases/17762-hyponatremia
- Skogestad J, Aronsen JM. Hypokalemia-Induced Arrhythmias and Heart Failure: New Insights and Implications for Therapy. Frontiers in Physiology. 2018;9. doi:https://doi.org/10.3389/fphys.2018.01500
- Tangvoraphonkchai K, Davenport A. Magnesium and Cardiovascular Disease. Advances in Chronic Kidney Disease. 2018;25(3):251-260. doi:https://doi.org/10.1053/j.ackd.2018.02.010
- Wu Z, Yang X, Ruan Z, Li L, Wu J, Wang B. Nonlinear relationship between dietary calcium and magnesium intake and peripheral neuropathy in the general population of the United States. Frontiers in Nutrition. 2023;10. doi:https://doi.org/10.3389/fnut.2023.1217465
- Castro D, Sharma S. Hypokalemia. National Library of Medicine. Published January 2025. https://www.ncbi.nlm.nih.gov/books/NBK482465/
- Camilleri M, Sellin JH, Barrett KE. Pathophysiology, Evaluation, and Management of Chronic Watery Diarrhea. Gastroenterology. 2017;152(3):515-532.e2. doi:https://doi.org/10.1053/j.gastro.2016.10.014
- Keely SJ, Barrett KE. Intestinal secretory mechanisms and diarrhea. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2022;322(4):G405-G420. doi:https://doi.org/10.1152/ajpgi.00316.2021
- Rangan GK, Dorani N, Zhang MM, et al. Clinical characteristics and outcomes of hyponatraemia associated with oral water intake in adults: a systematic review. BMJ Open. 2021;11(12):e046539. doi:https://doi.org/10.1136/bmjopen-2020-046539
- Peechakara BV, Gupta M. Water Toxicity. Nih.gov. Published September 30, 2019. https://www.ncbi.nlm.nih.gov/books/NBK537231/
- Balasundaram P, Santhanam P. Eating Disorders. National Library of Medicine. Published June 26, 2023. https://www.ncbi.nlm.nih.gov/books/NBK567717/
- Buh A, Scott M, Kiska R, et al. Impact of electrolyte abnormalities and adverse outcomes in persons with eating disorders: A systematic review protocol. PLoS ONE. 2024;19(8):e0308000-e0308000. doi:https://doi.org/10.1371/journal.pone.0308000
- Jiménez JV, Carrillo-Pérez DL, Rosado-Canto R, et al. Electrolyte and Acid–Base Disturbances in End-Stage Liver Disease: A Physiopathological Approach. Digestive Diseases and Sciences. 2017;62(8):1855-1871. doi:https://doi.org/10.1007/s10620-017-4597-8
- Berardi R, Torniai M, Lenci E, Pecci F, Morgese F, Rinaldi S. Electrolyte disorders in cancer patients: a systematic review. Journal of Cancer Metastasis and Treatment. 2019;2019. doi:https://doi.org/10.20517/2394-4722.2019.008
- Uppal N, Workeneh B, Rondon-Berrios H, Jhaveri K. Electrolyte and Acid-Base Disorders associated with Cancer Immunotherapy. Clinical Journal of the American Society of Nephrology. 2022;17(6):CJN.14671121. doi:https://doi.org/10.2215/cjn.14671121
- Cleveland Clinic. Rebalance, Replenish: 4 Sources of Electrolytes. Cleveland Clinic. Published September 22, 2023. https://health.clevelandclinic.org/best-electrolyte-sources
- National Institutes of Health. Office of Dietary Supplements - Potassium. Nih.gov. Published June 2, 2022. https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional/
- National Institute of Health. Calcium. Nih.gov. Published 2022. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
- Strazzullo P, Leclercq C. Sodium. Advances in Nutrition. 2014;5(2):188-190. doi:https://doi.org/10.3945/an.113.005215
- Medline Plus. Chloride in diet: MedlinePlus Medical Encyclopedia. Medlineplus.gov. Published 2018. https://medlineplus.gov/ency/article/002417.htm
- National Institute of Health. Office of Dietary Supplements - Magnesium. Nih.gov. Published 2017. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/
- Millard-Stafford M, Snow TK, Jones ML, Suh H. The Beverage Hydration Index: Influence of Electrolytes, Carbohydrate and Protein. Nutrients. 2021;13(9):2933. doi:https://doi.org/10.3390/nu13092933
- Cleveland Clinic. Dehydration. Cleveland Clinic. Published 2023. https://my.clevelandclinic.org/health/diseases/9013-dehydration
- Zhang Y, Coca A, Casa DJ, Antonio J, Green JM, Bishop PA. Caffeine and diuresis during rest and exercise: A meta-analysis. Journal of Science and Medicine in Sport. 2015;18(5):569-574. doi:https://doi.org/10.1016/j.jsams.2014.07.017
